What Is Anaphylaxis?
Reviewed by: HU Medical Review Board | Last reviewed: March 2022 | Last updated: February 2023
Living with allergies also carries the risk of anaphylaxis. Anaphylaxis is a severe, life-threatening allergic reaction that can be scary and traumatic to experience.1
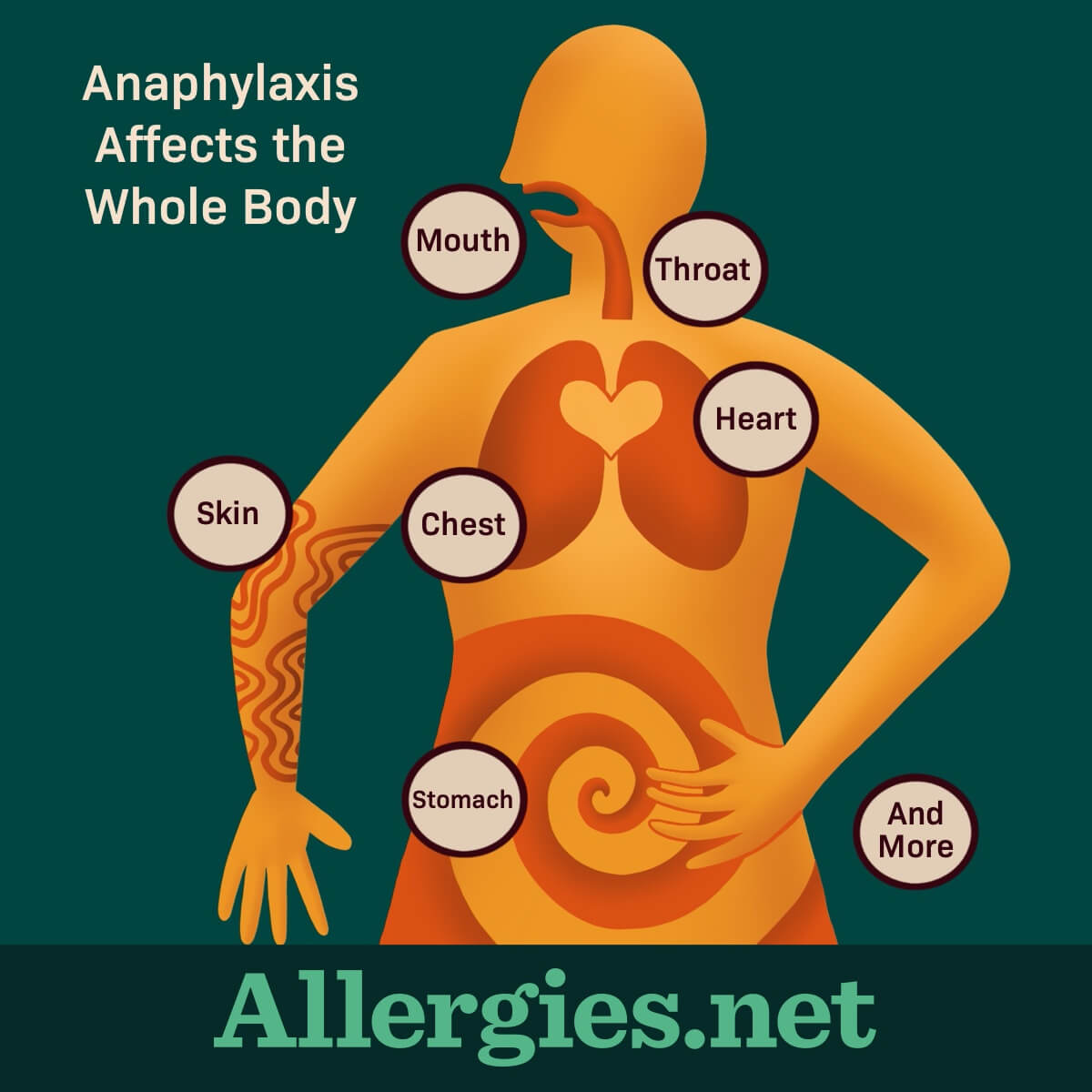
During anaphylaxis, the body strongly overreacts to the allergen, often affecting more than 1 system of the body at the same time. It requires quick action to reverse these symptoms. Usually, this means giving a dose of epinephrine immediately followed by a trip to the emergency room.1
Symptoms of anaphylaxis
Symptoms of anaphylaxis may occur quickly, often within minutes of exposure to the allergen. However, in some cases it can take even 30 minutes or more. Symptoms may affect different areas of the body and include:1-3
- Mouth – Itching, swelling of the lips and tongue
- Throat – Itching, swelling in throat, throat closing, hoarseness
- Skin – Itching, hives, redness, swelling, flushing
- Gut – Vomiting, diarrhea, cramping
- Lungs – Shortness of breath, wheezing, coughing
- Heart – Weak and rapid pulse, dizziness, fainting, pale or blue skin
- Other – Feeling something bad is about to happen, confusion
Sometimes symptoms start off mild, like a runny nose or a feeling that something is not right. These mild symptoms can quickly get much worse. Some areas of the body may have mild symptoms and other parts severe. Left untreated, anaphylaxis can be deadly.1-3
In some cases, a second anaphylactic reaction occurs without further exposure to the allergen. This is called a biphasic reaction. It can occur up to 12 hours after the first one.2
Who is most at risk?
Anaphylaxis can occur in nearly anyone who has an allergy, but some people may be more at risk than others.
People with allergies to certain foods, insect stings, certain drugs, and latex are more likely to have an anaphylactic reaction. In adults, the most common anaphylaxis triggers are drugs like antibiotics, aspirin, and insulin. In children, the most common triggers are foods.2,4
About 1.6 out of every 100 people in the United States may experience anaphylaxis during their lifetime. Research shows that rates of anaphylaxis seem to be increasing.5
If you have allergies or asthma and have a family history of anaphylaxis, you are also at higher risk for anaphylaxis yourself. People with uncontrolled asthma, especially teens and young adults, have a higher risk of severe anaphylactic reactions.5
Plus, if you have had anaphylaxis in the past, you are at higher risk of having another anaphylactic reaction.4
Your doctor can help you understand your risk for anaphylaxis. Ask about an anaphylaxis action plan and a prescription for epinephrine auto-injectors. Your doctor will show you how to use them.
How is anaphylaxis treated?
Treatment for anaphylaxis involves using an epinephrine auto-injector right away and calling 9-1-1. Many people with serious allergies carry 2 epinephrine auto-injectors at all times. This is because it may take 2 doses to control anaphylaxis symptoms.1
Once medical help arrives, you will likely be taken to a hospital for monitoring and any further treatment. Symptoms can come back or get worse, so it is important to go with the first responders to the hospital.1
The hospital may add other treatments to support epinephrine. This may include:6
- Oxygen to help with breathing
- Intravenous (IV) antihistamines and steroids, which can help reduce inflammation and hives
- Beta-agonist drugs like albuterol to treat breathing symptoms
If your heart stops or you stop breathing, cardiopulmonary resuscitation (CPR) may be needed.6
Can anaphylaxis be prevented?
While you may not be able to completely avoid anaphylaxis, you can take steps to reduce your risk of it happening. Some common tips include:1,7
- As much as possible, avoid any allergens you know trigger an allergic reaction.
- Know your allergens by getting an accurate diagnosis from an allergist.
- Be prepared in case you cannot avoid an allergen. Carry at least 2 epinephrine auto-injectors at all times and know how to use them.
- Tell friends and family about your allergy so they can help you avoid your triggers
- Have an anaphylaxis action plan.
- Talk with your doctor and caregivers about your allergies and what you can do to reduce your risk.
- Wear medical alert jewelry.
Things to know
Even if your allergies are mild or not the type to commonly trigger anaphylaxis, talk with your doctor about it. This discussion is even more important if you have a severe allergy.
Ask your doctor to explain the warning signs and symptoms of anaphylaxis. Develop an anaphylaxis action plan with your healthcare team. This will help prepare you for what to do in case of an emergency. You might never need to use the action plan – but if you do, at least the plan is in place.